- Alternative id - Pro00106301
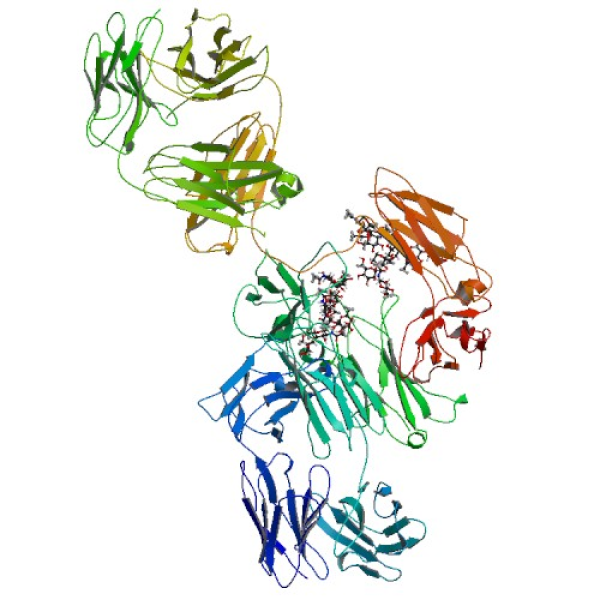
- Interventions - Drug: Infliximab|Drug: Abatacept|Drug: Remdesivir|Drug: cenicriviroc (closed to enrollment as of 3-Sep-2021)
- Study type - Interventional
- Study results - No Results Available
- Locations - Banner University Medical Center, Phoenix, Arizona, United States|University of Arkansas Medical Sciences, Little Rock, Arkansas, United States|Scripps Clinical Medical Group, La Jolla, California, United States|UCLA - Ronald Reagan Medical Center, Los Angeles, California, United States|Riverside University, Moreno Valley, California, United States|UC Irvine Medical Center, Orange, California, United States|Stanford University Medical Center, Palo Alto, California, United States|UCLA Medical Center- Santa Monica, Santa Monica, California, United States|Medstar Washington Hospital Center, Washington, District of Columbia, United States|University of Florida-Jacksonville, Jacksonville, Florida, United States|University of Illinois at Chicago, Chicago, Illinois, United States|Northwestern University, Chicago, Illinois, United States|Loyola University Medical Center, Maywood, Illinois, United States|University of Iowa, Iowa City, Iowa, United States|University of Kansas, Kansas City, Kansas, United States|University of Kentucky, Lexington, Kentucky, United States|Tulane School of Medicine, New Orleans, Louisiana, United States|University Medical Center New Orleans, New Orleans, Louisiana, United States|Ochsner Medical Center, New Orleans, Louisiana, United States|Anne Arundel Medical Center, Annapolis, Maryland, United States|Johns Hopkins Medical Center, Baltimore, Maryland, United States|Tufts Medical Center, Boston, Massachusetts, United States|Brigham and Women's Hospital, Boston, Massachusetts, United States|Boston Medical Center, Boston, Massachusetts, United States|Beth Israel Deaconess Medical Center, Boston, Massachusetts, United States|U Mass Memorial Medical Center, Worcester, Massachusetts, United States|U Mass University Medical Center, Worcester, Massachusetts, United States|MidMichigan Medical Center- Gratiot, Alma, Michigan, United States|MidMichigan Medical Center - Midland, Midland, Michigan, United States|Mayo Clinic, Rochester, Minnesota, United States|University of Mississippi Medical Center, Jackson, Mississippi, United States|University of Missouri Health Care, Columbia, Missouri, United States|Washington University School of Medicine, Saint Louis, Missouri, United States|Trinitas Hospital, Elizabeth, New Jersey, United States|Hackensack University Medical Center, Hackensack, New Jersey, United States|Rutgers New Jersey Medical School, New Brunswick, New Jersey, United States|NYU Brooklyn, Brooklyn, New York, United States|University at Buffalo, Buffalo, New York, United States|Flushing Hospital Medical Center, Flushing, New York, United States|Jamaica Hospital Medical Center, Jamaica, New York, United States|NYU Long Island, Long Island City, New York, United States|New York University Langone Medical Center, New York, New York, United States|Harlem Hospital Center, New York, New York, United States|Weill Cornell Medicine, New York, New York, United States|St Lawrence Health System, Potsdam, New York, United States|University of Rochester Medical Center-Strong Memorial Hospital, Rochester, New York, United States|University of North Carolina - Chapel Hill, Chapel Hill, North Carolina, United States|Duke University, Durham, North Carolina, United States|Wake Forest University, Winston-Salem, North Carolina, United States|Mercy Saint Vincent Medical Center, Toledo, Ohio, United States|University of Oklahoma Health Sciences Center, Oklahoma City, Oklahoma, United States|Oregon Health and Science University, Portland, Oregon, United States|Temple University Hospital, Philadelphia, Pennsylvania, United States|Reading Hospital Study, Wyomissing, Pennsylvania, United States|Avera McKennan Hospital, Sioux Falls, South Dakota, United States|University of Tennessee Medical Center, Knoxville, Tennessee, United States|Methodist Health System Clinical Research Institute, Dallas, Texas, United States|University of Texas Health Science Center - Houston, Houston, Texas, United States|University of Texas Health Science Center at San Antonio, San Antonio, Texas, United States|Trinity Mother Frances Hospital, Tyler, Texas, United States|University of Texas Health Center at Tyler, Tyler, Texas, United States|University of Utah, Salt Lake City, Utah, United States|Virginia Commonwealth University Medical Center, Richmond, Virginia, United States|University of Washington Medical Center, Seattle, Washington, United States|Providence Medical Research Center, Spokane, Washington, United States|West Virginia University, Morgantown, West Virginia, United States|Gundersen Health System, La Crosse, Wisconsin, United States|Hospital Interzonal Dr Jose Penna Bahia Blanca, Bahía Blanca, Buenos Aires, Argentina|Sanatorio Ramon Cereijo, Caba, Buenos Aires, Argentina|Instituto Medico Platense, La Plata, Buenos Aires, Argentina|Clinica Central S.A., Villa Regina, Rio Negro, Argentina|Hospital Ramos Mejia, Buenos Aires, Argentina|Hospital Rawson, Cordoba, Argentina|Sanatorio Allende, Córdoba, Argentina|Sanatorio Britanico, Rosario, Argentina|Sanatorio Diagnóstico/ Instituto del Buen Aire, Santa Fe, Argentina|Hospital Brasília, Brasília, DF, Brazil|Hospital Felício Rocho, Belo Horizonte, MG, Brazil|Instituto DOR de Ensino e Pesquisa Hospital Glória D'Or, Rio De Janeiro, Rio De Janeiro / RJ, Brazil|Hospital Ernesto Dornelles, Porto Alegre, Rio Grande D Sul /RS, Brazil|Hospital de Clinicas de Porto Alegre HCPA, Porto Alegre, Rio Grande Do Sul / RS, Brazil|Santa Casa de Misericordia de Porto Alegre, Porto Alegre, Rio Grande Do Sul/RS, Brazil|Hospital e Maternidade Celso Pierro - PUC Campinas, Campinas, São Paulo/SP, Brazil|Nuevo Hospital Civil de Guadalajara "Dr. Juan I. Menchaca", Guadalajara, Guadalajara Jalisco, Mexico|Hospital Universitario "Dr. Jose Eleuterio Gonzalez", Nuevo León, Monterrey, Mexico|Hospital Central FAP, Lima, Lima/Lima, Peru|Hospital Regional Lambayeque, Chiclayo, Peru|Hospitala Nacional Hipólito Unánue, Lima, Peru|Hospital Nacional Aezobispo Loayza, Lima, Peru|Hospital de Chancay y Servicios Basicos de Salud, Lima, Peru|Clínica Belén SANNA, Piura, Peru
- Study designs - Allocation: Randomized|Intervention Model: Parallel Assignment|Masking: Triple (Participant, Investigator, Outcomes Assessor)|Primary Purpose: Treatment
- Enrollment - 1971
- Age - 18 Years and older (Adult, Older Adult)
- Outcome measures - Number of patients that recovered from COVID-19|Change in number of patients hospitalized on invasive mechanical ventilation|number of patients that improved clinically|Number of patient deaths|Number of patients with decreased supplemental oxygenation needed|Change in number of patients needing non-invasive ventilation/ high flow oxygen|Number of days patients are in the hospital|Number of SAEs and AEs of grade 3 and 4|Number of patients with changes in abnormal WBC counts
|